What if training your immune system to attack cancer cells was as easy as training it to fight Covid-19? Many people believe the technology behind some Covid-19 vaccines, messenger RNA, holds great promise for stimulating immune responses to cancer.
But using messenger RNA, or mRNA, to get the immune system to mount a prolonged and aggressive attack on cancer cells — while leaving healthy cells alone — has been a major challenge.
The MIT spinout Strand Therapeutics is attempting to solve that problem with an advanced class of mRNA molecules that are designed to sense what type of cells they encounter in the body and to express therapeutic proteins only once they have entered diseased cells.
“It’s about finding ways to deal with the signal-to-noise ratio, the signal being expression in the target tissue and the noise being expression in the non-target tissue,” Strand CEO Jacob Becraft PhD ’19 explains. “Our technology amplifies the signal to express more proteins for longer while at the same time effectively eliminating the mRNA’s off-target expression.”
Strand is set to begin its first clinical trial in April, which is testing a self-replicating mRNA molecule’s ability to express immune signals directly from a tumor, triggering the immune system to attack and kill the tumor cells directly. It’s also being tested as a possible improvement for existing treatments to a number of solid tumors.
As they work to commercialize its early innovations, Strand’s team is continuing to add capabilities to what it calls its “programmable medicines,” improving mRNA molecules’ ability to sense their environment and generate potent, targeted responses where they’re needed most.
“Self-replicating mRNA was the first thing that we pioneered when we were at MIT and in the first couple years at Strand,” Becraft says. “Now we’ve also moved into approaches like circular mRNAs, which allow each molecule of mRNA to express more of a protein for longer, potentially for weeks at a time. And the bigger our cell-type specific datasets become, the better we are at differentiating cell types, which makes these molecules so targeted we can have a higher level of safety at higher doses and create stronger treatments.”
Making mRNA smarter
Becraft got his first taste of MIT as an undergraduate at the University of Illinois when he secured a summer internship in the lab of MIT Institute Professor Bob Langer.
“That’s where I learned how lab research could be translated into spinout companies,” Becraft recalls.
The experience left enough of an impression on Becraft that he returned to MIT the next fall to earn his PhD, where he worked in the Synthetic Biology Center under professor of bioengineering and electrical engineering and computer science Ron Weiss. During that time, he collaborated with postdoc Tasuku Kitada to create genetic “switches” that could control protein expression in cells.
Becraft and Kitada realized their research could be the foundation of a company around 2017 and started spending time in the Martin Trust Center for MIT Entrepreneurship. They also received support from MIT Sandbox and eventually worked with the Technology Licensing Office to establish Strand’s early intellectual property.
“We started by asking, where is the highest unmet need that also allows us to prove out the thesis of this technology? And where will this approach have therapeutic relevance that is a quantum leap forward from what anyone else is doing?” Becraft says. “The first place we looked was oncology.”
People have been working on cancer immunotherapy, which turns a patient’s immune system against cancer cells, for decades. Scientists in the field have developed drugs that produce some remarkable results in patients with aggressive, late-stage cancers. But most next-generation cancer immunotherapies are based on recombinant (lab-made) proteins that are difficult to deliver to specific targets in the body and don’t remain active for long enough to consistently create a durable response.
More recently, companies like Moderna, whose founders also include MIT alumni, have pioneered the use of mRNAs to create proteins in cells. But to date, those mRNA molecules have not been able to change behavior based on the type of cells they enter, and don’t last for very long in the body.
“If you’re trying to engage the immune system with a tumor cell, the mRNA needs to be expressing from the tumor cell itself, and it needs to be expressing over a long period of time,” Becraft says. “Those challenges are hard to overcome with the first generation of mRNA technologies.”
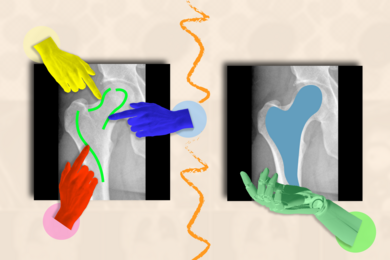
Strand has developed what it calls the world’s first mRNA programming language that allows the company to specify the tissues its mRNAs express proteins in.
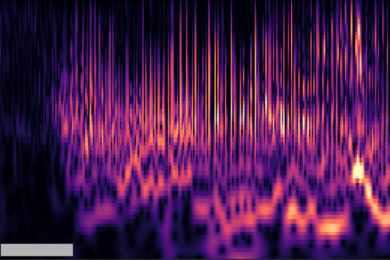
“We built a database that says, ‘Here are all of the different cells that the mRNA could be delivered to, and here are all of their microRNA signatures,’ and then we use computational tools and machine learning to differentiate the cells,” Becraft explains. “For instance, I need to make sure that the messenger RNA turns off when it's in the liver cell, and I need to make sure that it turns on when it's in a tumor cell or a T-cell.”
Strand also uses techniques like mRNA self-replication to create more durable protein expression and immune responses.
“The first versions of mRNA therapeutics, like the Covid-19 vaccines, just recapitulate how our body’s natural mRNAs work,” Becraft explains. “Natural mRNAs last for a few days, maybe less, and they express a single protein. They have no context-dependent actions. That means wherever the mRNA is delivered, it’s only going to express a molecule for a short period of time. That’s perfect for a vaccine, but it’s much more limiting when you want to create a protein that’s actually engaging in a biological process, like activating an immune response against a tumor that could take many days or weeks.”
Technology with broad potential
Strand’s first clinical trial is targeting solid tumors like melanoma and triple-negative breast cancer. The company is also actively developing mRNA therapies that could be used to treat blood cancers.
“We’ll be expanding into new areas as we continue to de-risk the translation of the science and create new technologies,” Becraft says.
Strand plans to partner with large pharmaceutical companies as well as investors to continue developing drugs. Further down the line, the founders believe future versions of its mRNA therapies could be used to treat a broad range of diseases.
“Our thesis is: amplified expression in specific, programmed target cells for long periods of time,” Becraft says. “That approach can be utilized for [immunotherapies like] CAR T-cell therapy, both in oncology and autoimmune conditions. There are also many diseases that require cell-type specific delivery and expression of proteins in treatment, everything from kidney disease to types of liver disease. We can envision our technology being used for all of that.”